Yet Another Inquest Into the Land of “Functional” vs. “Non-functional”
Guest post by Jarred Boyd, PT, DPT, MSAT, Director of Rehabilitation for the Memphis Grizzlies
Over the years, contention has existed, and will likely persist into the foreseeable future, revolving around what is and is not considered functional. While one could argue that we, as “movement professionals”, should direct our attention to more essential problems, I would contest, particularly in the rehabilitation landscape, the dichotomy of functional vs. non-functional remains an essential issue.
Remaining shackled to our convictions precludes us from receiving credible insights and cloaks us in a false sense of current certainty – a facade of pride and ego. To expand our clinical insight perhaps we should approach the profession as a pendulum – moving away from midline with the intention of attaining differing beliefs, eventually coming back to the middle – converging the divergent experiences, information, and data with our current beliefs. More importantly, resolving the unproductive clashing of ideologies held between functional and non-functional “tribes” may positively influence athlete/patient outcomes, a pursuit we are each striving toward.
Current pitfalls of “functional”
“Functional” is often based on the extent to which a movement demonstrates dynamic correspondence and representativeness of the sport specific task. Conversely, “non-functional” is frequently deemed as a movement which fails to demonstrate the exact kinematics/positions of the sport/task or significantly reduces the athlete’s degrees of freedom. For example, clinicians may consider back squats owning superior functionality for the restoration of quadriceps force generation capacity, or even structural adaptations (i.e., hypertrophy), while neglecting the utility of leg extensions.
A lack of consensus for the definition of “functional” may lead practitioners to dismiss exercises that could resolve physical performance deficits and/or reject implementation of isolated testing during a reconditioning process. Therefore, establishing a definition may help fuel critical thinking when it comes to clinicians determining the usefulness of various training solutions and capacity tests. By adopting the perspective that exercises which mimic sport are fundamentally more functional, practitioners may at times yield a low return on investment and underdeliver key stimuli necessary for specific adaptations.
This lack of consensus for the definition of functional may lead practitioners toward dismissing exercises that could resolve physical performance deficits.
Defining “functional”
My operational definition for “functional”, which is surely flawed, is: Any activity that reduces constraints and enhances boundaries, increasing the potential to improve performance of a task. By subscribing to this definition, one may appreciate why a training solution may not have to replicate the exact kinematics/strategy of that produced during the sporting task. Sporting tasks are incredibly reflexive and reactive, or better put, emergent – especially in field and court sports. They are influenced by the self- organization of available capacities and capabilities owned by the athlete.
Attempting to recreate the exact positions in sport may result in under preparation of tissue-specific strength and neuromuscular systems capacities as we fail to ensure sufficient load to relevant tissues has been delivered. The possession of requisite tissue-specific force generating capacities or stress-strain capacity to “handle” a preferential strategy may afford protection and promote performance.
Exercises that mimic the sport are neither more nor less functional than exercises that do not mimic the sport – as any exercise that serves as a vehicle for the relevant adaptations should be considered functional.
Establishing key determinants of the task
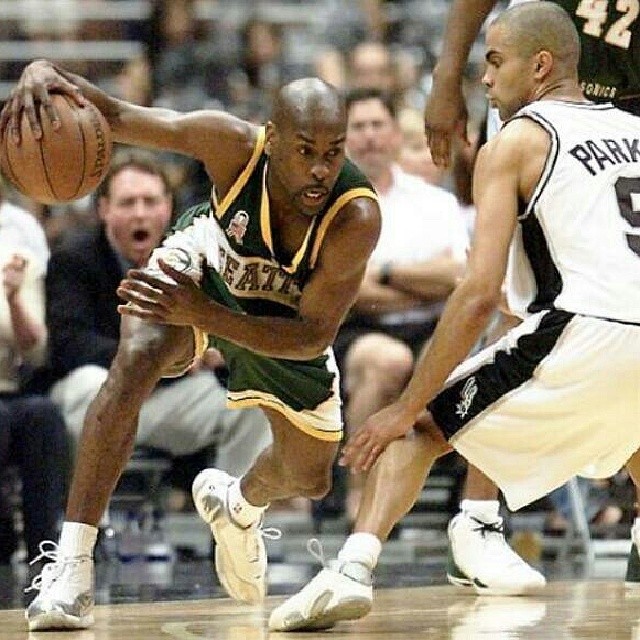
Analyzing the dynamic actions that athletes perform in sport may be more important for understanding the specific tissues and neuromuscular capacities required. As a result, practitioners may feel empowered to select the most relevant training solutions – despite how closely it does or does not resemble the sporting task. Understanding the relevant sport demands provides critical insight in what distinct capacities or general capabilities particular actions mandate. For example, when assessing the sport of basketball, a primary intent is to invade an opponent’s space to prevent them from scoring or to evade a defender to create separation for a less impeded shot attempt.
Whether assessing invasion or evasion, both actions fundamentally necessitate the redirection of one’s motion (change of direction) by the application of force over a specific time period (impulse). This prompts us to appreciate how momentum (velocity x mass) must be manipulated (deceleration), requiring sufficient force generating capacities to handle large braking forces. Expanding the involved tissue’s envelope of function with constrained isolated (e.g., isokinetic leg extension) and integrated loading (e.g., leg press), via differing masses and velocities, may support an athlete’s tissue structure and neuromuscular capacities to contend with mechanical forces during sport.
Observing the above pictures and claiming it is mandatory to implement training that specifically puts athletes in the same position because it is “functional” may lead to immature capacities. Instead, acknowledging the kinetics (force magnitude and direction) and appreciating the resulting kinematics (position of the body in relation to itself) would provide insight into the tissues that could, for example, benefit from maximal force production (peak) and explosive force production (rate) capacities.
Exercises that mimic the sport are neither more nor less functional than exercises that do not mimic the sport – as any exercise that serves as a vehicle for the relevant adaptation(s) shoulder be considered functional.
Increasing isolated tissue capacity may promote protection by expanding not only an athlete’s threshold of mechanical failure but also their performance potential. However, one’s performance potential, or available movement options, may be narrow if an isolated tissue’s neuromuscular determinants of force are reduced.
This is especially apparent after injury where residual deficits are often present, calling upon alternate regions to assist in force generation. If specific tissues fail to recover their capacities this may be a bottleneck in the athlete’s success, potentially increasing susceptibility to stress-strain exceeding forces.
When establishing key determinants of a task, we are attempting to highlight the essential ingredients of the final adaptations. Thereafter, we can devise effective isolated training solutions without being confined to solely movements that mirror said sporting task. Expanding these isolated force generating capacities may increase the movement solutions available to solve movement questions. Additionally, expanding the isolated force generating capacities may help spread the distribution of work – a potentially favorable solution for moderating focal tissue stress.
We may expand the available movement solutions to solve movement questions by broadening an athlete’s range of force generating capacities.
Testing and training key determinants of the task
Due to movement variability, unconstrained tasks may fail to identify if a specific joint has resolved key physical capacities. Let’s use the final stages of anterior cruciate ligament reconstruction (ACL-R) rehab. A commonly used physical metric identifying successful reconditioning after ACL-R is single limb hop testing, a dynamic output. As rapid single leg loading is an action performed in several sports there is a widely held belief that hop testing is most representative of an athlete’s performance potential – or more commonly touted, hop testing is more “functional”. Although this conclusion is well-intended, it shackles our ability to navigate and appreciate potential constraints.
Hop performance, typically measured via distance asymmetry, will fail to reveal individual components of kinetic limb capacity and asymmetry and may ultimately serve as a misplaced proxy for performance restoration. The prioritization of hop testing is merely one of the many problematic scenarios that may result in compensatory solutions, which is typically an expression of underdeveloped internal knee extensor force generating capacity.
Constraining tests and tasks can assist in detecting if specific force generating capacities are available, minimizing the potential of false negatives (missing the presence of issues). This constraints-based assessment may highlight the potential rate limiting qualities that have higher merit for resolving. As a result, we may select a more applicable training solution to reverse the relevant trainable deficits.
Using the ACL-R example again, establishing a sensible hierarchy of needs throughout the reconditioning process will help us avoid our own deception from hop testing symmetry. Hop testing may, and often will, reflect numerous movement strategies. Athletes will commonly use a subconscious strategy involving the hip and ankle to achieve symmetrical distance or manipulate the time spent in contact with the ground. Hence the use of mechanical muscle function measures via both isolated (e.g., leg extension dynamometry) and integrated (e.g., leg press) testing may increase the odds of selecting the most relevant training solutions resolving trainable deficits, without succumbing to the contentious debate of whether the exercise or test is “functional”.
Removing the various movement options that athletes adopt during dynamic tests may increase our ability to detect if isolated capacities are restored.
By-passing constrained testing in favor of only unconstrained testing may increase the probability of inaccurately detecting the deficit as all the ingredients are now mixed. Before a constrained force generating capacity may be rectified, one must first determine via testing what specific quality needs intervening. Capacity testing, particularly earlier in the reconditioning process, is purposefully meant to be sterile and controlled rather than imitating each movement performed during the chaotic nature of sport. The intent is to assess whether there has been a resolution of the specific trainable deficits that could constrain the athlete’s performance potential. Essentially, we are asking if the ingredients are even available to make the end recipe.
There are too many strategies which an athlete can construct and demonstrate “success”, even without a particular ingredient. However, this may simply create a narrower boundary of available solutions. The expression of a quality during a sporting task should not always imply that the sporting task is inherently sufficient (i.e., more “functional”) at adapting said quality, particularly when it comes to reconditioning of specific capacities.
Constrained testing may help determine if requisite ingredients are available for the final recipe.
Let’s continue to analyze this from the perspective of ACL-R. I think here we would find that many clinicians would have preference toward squatting over leg extensions as the most effective loading option during rehab. Now, while there is nothing inherently wrong with squatting, leg extensions may reduce the potential for intra-limb/inter-joint compensations where the tissues around hip and ankle joints contribute to more impulse than the knee. In addition, squatting, without sufficient internal knee extension moment, may also result in inter-limb compensation where the athlete offloads the injured limb.
This reduces the mechanical tension that is a necessary hypertrophic signal to adapt the quadriceps and may allow or potentiate future asymmetries. In this scenario, I view leg extensions as being akin to a traffic cop: Directing traffic which may help improve the flow of traffic to specific streets much like directing a stimulus toward specific tissues.
Both loading options are “functional”, however, that is dependent on the adaptations one desires and if the loading option targets the specific components underlying the adaptation.
Final thoughts…
By having too many components to an exercise, sometimes it can be too much “noise”. Or better put, you are implementing too many components at once and you end up negatively impacting the intended route of the stimulus, failing to adapt said quality. Perhaps we can view this like removing or adding bowling bumpers; the intention is to increase the probability of the stimulus reaching the intended target for a specific end outcome. However, many times we approach the reconditioning process under the guise of a false narrative – wrongly thinking that we should omit all bumpers (i.e., constrained + isolated loading) as it is more “functional”.
Now of course, there is NO single right answer. However, intentionally rethinking our beliefs and remaining open, yet healthily skeptical, to alternative perspectives (which require both humility and curiosity) may encourage deeper clinical appraisal.
With this said, we can and should implement both constrained isolated and unconstrained integrated exercise variants, essentially running a sort of concurrent reconditioning model, ensuring the unconstrained exercise/drill does not exceed the current tissue’s capacity. Appreciating the relevance of constrained isolated training solutions may foster clinical adaptability, an essential character trait for clinicians to hold throughout the dynamic process of rehabilitation/reconditioning.
In other words: Worry less about what is “functional” and more about the key determinants of the final adaptation.
You can reach Jarred on Instagram.
Figure 1 is “Olympic friendly” by GPA Photo Archive from Flickr
Figure 2 is “Gary Payton – Seattle Supersonics. Oakland Skyline High School” by Russell Mondy from Flickr