Movement Overdiagnosis in Physical Therapy – Why Less is Usually More
First, a Physical Therapy Haiku…
Posture picked apart
every pain a syndrome named
motion lost to fear.
I am a product of the videocassette recorder (VCR). I watched an average of 3 movies a week on the VCR during my adolescence and early adulthood. In Physical Therapy School, I worked at the local video store and tried to impress my classmates with my access to “screeners”. These were early releases, a month before the actual VHS tape of a particular blockbuster would be available to the public. From 1983 to 1999, I’m Your Huckleberry in movie trivia. But alas, now we have IMDB and Rotten Tomatoes. Frankly, you also have the World Wide Web, which only appeared publicly in 1994, when I started PT school.
I could spend this blog post discussing Tombstone (released to theaters on Christmas Day, 1993), starring Kurt Russell and Val Kilmer. If you haven’t seen it, you should. That’s my movie recommendation for this post.
If you have ever been to Tombstone, AZ, a big tourist attraction is Boot Hill. Touring the cemetery, you will see Lester Moore’s tombstone in Row 6. Lester Moore worked for the Wells Fargo office in Naco, AZ, and one day Hank Duston came in and was pissed off about how his package was damaged. He shot Lester four times, but Lester was able to get a shot off, and both men died that day. Lester’s epitaph is one of the most famous ones in Boot Hill…
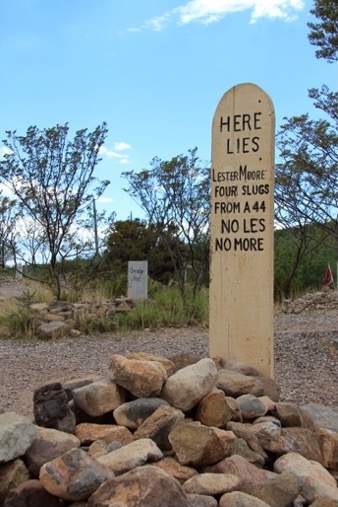
When I hear “less is more,” I immediately think of Lester Moore. It’s likely tied to the same brain wiring that allows spontaneous dad jokes. Regardless, I thought of “less is more” and “Lester Moore” when I saw the recent article in JAMA Internal Medicine about the impact of disease definitions on overdiagnosis. The article is interesting; my takeaway was how the PT profession has a similar issue in our posture and movement definitions.
The “less is more” philosophy holds especially true when applied to the external facets of our lives – chasing the latest fashion trends, doom-scrolling social media, indulging in gourmet foods, or spending on nonessential items. In my case, I should focus less on the amount of Starbucks® rewards I have and also reduce the number of hazy IPAs I drink, albeit, “In Vino Veritas.” Many people focus too heavily on earning more money, rather than effectively managing what they already have. True financial freedom and lasting wealth come from living below your means and prioritizing intentional simplicity over excess. “Less is more” also applies to what we do when we enter the clinic on a workday.
Physical Therapists like to label stuff. This is secondary to our struggle and good intentions to relieve a patient’s pain. We want to alleviate their suffering, but we don’t know what is causing their pain. So, we turn to a common denominator and patsy: a pathological movement diagnosis.
Movement overdiagnosis in physical therapy (PT) refers to the excessive labeling or pathologizing of normal or minor variations in human movement, often leading to unnecessary treatment, fear, or altered behavior in patients. It’s a form of overmedicalization where therapists identify “problems” in movement that may not cause harm or contribute to the patient’s pain or dysfunction.
The concept of “less is more” in physical therapy (PT) reflects a shift toward efficiency, evidence-based practice, and patient-centered care. Minimal, targeted intervention often leads to better outcomes than excessive treatment.
What “Less is More” Means in PT
- Minimal Effective Dose
- Rather than overloading patients with complex routines, clinicians focus on prescribing the fewest necessary interventions that still yield meaningful progress.
- This might mean one or two high-impact exercises instead of a list of ten.
- Avoiding Overtreatment
- Modalities like ultrasound, electrical stimulation, or prolonged passive treatments (e.g., manual therapy without active exercise) often offer little long-term benefit.
- The “less is more” principle encourages avoiding low-value treatments, especially when they can increase cost or dependency.
- Reducing Dependency
- Empowering patients through education, self-management strategies, and movement confidence often reduces the need for long-term supervised care.
- Over-reliance on therapist-guided sessions can sometimes inhibit recovery.
- Embracing Simplicity in Movement
- PTs increasingly recognize that perfect form isn’t always necessary, and that natural variation in movement is normal and healthy.
- Simplifying goals and accepting “good enough” function can prevent fear-avoidant behavior and overcorrection.
Clinical Examples
- Chronic Low Back Pain:
- Instead of long-term passive care, many benefit more from education, graded activity, and reassurance. Often, a few targeted movements plus confidence-building are more effective than months of hands-on treatment.
- Tendinopathy:
- Eccentric or isometric loading—done consistently and simply—outperforms complicated multimodal strategies.
The benefits of a “less is more” approach include encouraging autonomy and self-efficacy, reducing over-medicalization and fear, saving time and cost for patients, improving adherence and functional outcomes, and aligning with current best-practice guidelines.
“Less is more” in PT doesn’t mean doing nothing—it means doing the right things at the right time and amount. It’s about clinical precision, not excess. Finally, as always, I could be mistaken. If so, write your own blog post. “You’re A Daisy If You Do.”
More reading
- Maher CG, O’Keeffe M, Buchbinder R, Harris IA. Musculoskeletal healthcare: Have we over-egged the pudding? Int J Rheum Dis. 2019;22:1957–1960.
- O’Keeffe M, Michaleff ZA, Harris IA, et al. Public and patient perceptions of diagnostic labels for non-specific low back pain: a content analysis. Eur Spine J. 2022;31:3627–3639.
- O’Keeffe M, O’Sullivan P, Purtill H, Bargary N, O’Sullivan K. Cognitive functional therapy compared with a group-based exercise and education intervention for chronic low back pain: a multicentre randomised controlled trial (RCT). Br J Sports Med. 2020;54:782–789.
- Zadro JR, O’Keeffe M, Ferreira GE, et al. Diagnostic Labels for Rotator Cuff Disease Can Increase People’s Perceived Need for Shoulder Surgery: An Online Randomized Controlled Experiment. J Orthop Sports Phys Ther. 2021;1–45.
About the Author

J.W. Matheson is a physical therapist with 30 years of experience and a growing passion for making science accessible to everyday people. Over the years, he’s learned that physical therapy—and the research behind it—isn’t the neat, airtight world textbooks promise. Musculoskeletal pain science is messy, flawed, and deeply human, just like the people it aims to help.
While many talk about “evidence-based” practice, J.W. leans toward science-based practice—grounded in the best available research, scientific reasoning, healthy skepticism, solid methodology, and an understanding of where the evidence falls short. Once a fiery debater on social media, J.W. found that arguing rarely changes minds. Now, he’s more interested in listening than lecturing, asking better questions than delivering quick answers. He believes the best PTs aren’t the ones who are always “right,” but the ones who stay open, curious, and compassionate in the face of uncertainty. Through his writing, J.W. invites others to explore the gray areas of healthcare, where humility meets science—and where true progress happens.
Featured image is Grave of Lester Moore by Andamanse on Dreamstime.com
