Special Tests Can Be Special
Healthcare providers have a love/hate relationship with orthopedic special tests. Some seem to be really useful while others seem not to hold up very well to scrutiny. Much of these conversations seem to focus on the accuracy of any given test, typically in the language of sensitivity and specificity.
I think one of the issues that we come up against is that the accuracy of many of these tests lies in the interpretation. If you want your accuracy to improve with many of these tests, I feel that practicing some “interpretation discipline” can go a long way.
Interpretation discipline is holding your interpretation in check regarding the findings of any special test. Keep your interpretations extremely narrow and specific to the details of the test.
Often when I would teach a special test at a weekend course, I would get this question over and over again: “What does it mean if this test is positive?”
And my response would be: “Assuming you did it properly, it just means that the test is positive.”
Let me explain. First, let’s break these special tests into two major categories: Integrity and Pain-Provoking.
Integrity special tests
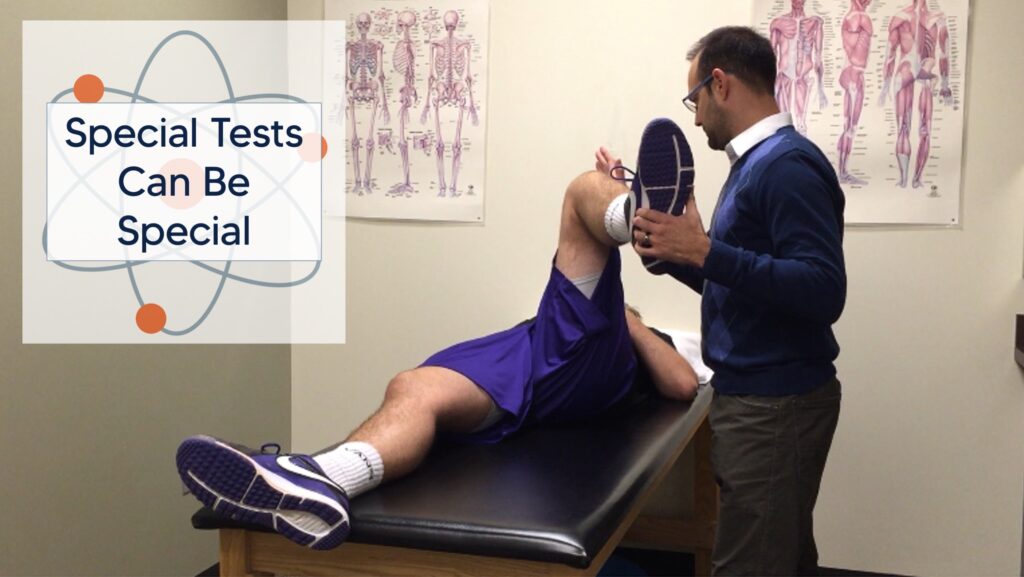
Integrity special tests would be our tests that assess the integrity of a joint without using the subjective report of the patient as part of the assessment. These are tests that assess the structures that provide physical integrity to a joint like ligaments and labrums. A classic example would be the Lachman test for an ACL injury.
First, I have to have good prior probability that makes performing the test useful in the first place (that’s a blog post that I’ve already written). Assuming that I have that, if I find extreme differences between the uninvolved knee and the involved knee, I personally have pretty high confidence in a Lachman test.
In other words, if I feel a firm, short, and snappy endfeel on the uninvolved side and a huge amount of movement with no endfeel on the involved side, I’m probably looking at a torn ACL. Conversely, if I feel an equally firm, short, and snappy endfeel bilaterally, I’m pretty confident that I’m probably not looking at a torn ACL. Notice the use of the word “probably” in both situations.
If I find anything else, like short play with no snappy endfeel or subtle differences in translation, I simply deem the test “inconclusive” and move on.
Other examples would be macro-instability tests like load-and-shift and the jerk tests at the shoulder. These tests where you have frank passive movement asymmetry often correlate fairly well to gold standards like MRI or surgical observation. The more objective you keep the tests the better. If you start to “grade” them, it would make sense that you are raising your likelihood of being wrong. Just keep your scoring to “clearly positive”, “clearly negative”, or “inconclusive” and you should be ok.
Pain-provoking special tests
Pain-provoking special tests are tests that place the patient’s body into certain positions and ask, “Does that hurt?” There are …a lot… of these tests. This includes most impingement tests of the hip and shoulder (Neer’s, Hawkins/Kennedy, FADIR, etc), those “grind” tests of the knee (McMurray’s, Clarke’s sign, etc), plus many others.
The biggest problem with these pain-provoking tests is when you try to make structural diagnoses around them. The Hawkins/Kennedy test does not assess whether or not your patient has impingement; actually if your patient has a shoulder then they have impingement. The compression-rotation test (O’Brien’s test) does not tell you whether or not they have a SLAP lesion; plenty of people have SLAP lesions without symptoms. Just like meniscus tears.
Interpreting pain-provoking tests
So are they useful? I would say that they are absolutely useful! Just not to make a structural diagnosis. There are three possible interpretations you can draw from any of these tests:
- Clearly positive test = Putting their body in this position is clearly painful for the patient
- Clearly negative test = Putting their body in this position is clearly not painful for the patient
- Meh (some discomfort but not terrible) = Inconclusive.
Even though this does not give you a structural diagnosis, this gives you a nice description of their presentation. If you would like to be even more objective, use a handheld dynamometer for conducting these tests. Now you can tell how much force it takes to correlate to pain. This is something that you can now track if you so choose. I usually don’t unless it is specifically a position that this individual needs for function (depends on the patient). For example, a patient may solve their shoulder dysfunction by just avoiding the painful position. The test doesn’t need to change.
But the results of these tests do inform your plan of care. For example, a cluster of positive shoulder impingement signs (clinical exam/tests) and symptoms (subjective report) gives you a quick idea of the kinds of exercises that they should tolerate well and which ones you may want to avoid initially.
Whether or not someone has a meniscus tear doesn’t matter. Whether or not they are tolerating their knee pain does matter, regardless of the presence of a meniscus tear. The simple goal of physical therapy in these population is to help the patient become more tolerant of the demands of their desired functional tasks.
In summary…
- Special tests are useful as long as you don’t overthink them
- Practicing “interpretation discipline” is necessary
- Prior probability must always be considered
- Integrity tests can be more objective about structure than pain-provoking tests
- Even if a test tells you little that is useful about the underlying structure, they can tell you something about your patient’s situation